Abstract
BACKGROUND Haploidentical donor (HID) transplantations have achieved comparable survival as HLA fully matched unrelated donor (URD) transplantations. However, previous studies usually consider the two donor sources as whole populations when making the comparison, although there are actually subgroups within each. Based on current knowledge regarding donor selection, offspring and sibling donors were prioritized over parental donors in unmanipulated haplo-transplant settings, and maternal donors were considered as "the worst donors" under the Beijing Protocol due to the increased probabilities of GVHD and inferior survival. To compare efficacies of "the worst" mother donors and URDs would help to acquire a further understanding on donor selection of HIDs versus URDs.
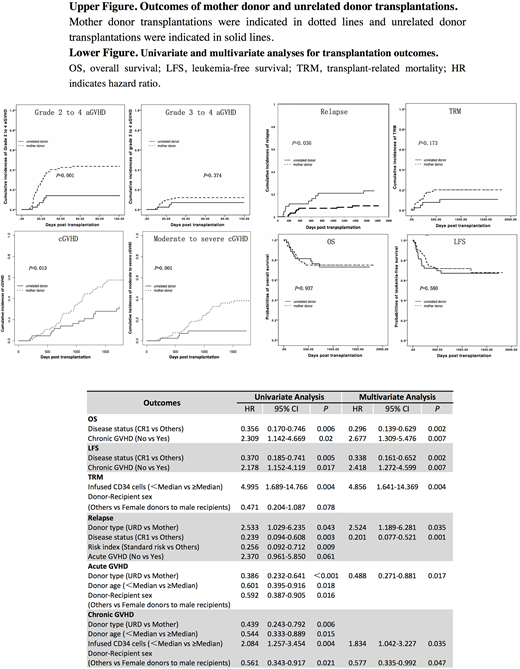
PATIENTS AND METHODS 43 and 92 patients who underwent transplantations with URDs or mother donors from June 2012 to June 2015 were enrolled. Their transplantation outcomes, including hematopoietic recovery, acute and chronic GVHD, relapse, transplant related mortality (TRM), overall survival (OS) and leukemia-free survival (LFS) were compared. Univariate and multivariate analysis were performed to explore risk factors for transplantation outcomes.
RESULTS Both 2-year OS and 2-year LFS were comparable between the mother donor group and the URD group (74.8% versus 72.9%, p=0.937 and 71.7% versus 67.0%, p=0.580). Higher incidences of grade 2 to 4 acute GVHD and chronic GVHD were observed in the mother donor group than that in the URD group (43.5% versus 14.0%, p=0.001 and 58.8% versus 37.1%, p=0.013), although incidences of grade 3 to 4 aGVHD were similar between groups (mother donor group: 12%, URD group: 7%, p=0.374). Multivariate analysis indicated increased rates of acute GVHD were associated with mother donor transplantations (HR ratio: 2.049, p=0.017) and chronic GVHD was related to lower dose of CD34 cells infused (HR ration: 1.834, p=0.035) and female to male donations (HR ration: 1.733, p=0.047). The 2-year cumulative incidences of relapse were significantly decreased in the mother-donor group (7.6% versus 20.9%, p=0.036). Incidences of relapse were associated with donor types (URD vs mother donor: HR ratio 2.524, p=0.035) and disease status before transplantation (CR1 vs other: HR ratio 0.201, p=0.001) in multivariate analysis. These two groups were comparable in hematopoietic recovery and TRM (mother donor group: 21.1%, URD group: 11.6%, p=0.173).
CONCLUSIONS Our findings suggest that mother donor transplantations could achieve comparable survival to unrelated donor transplantations, and exhibited decreased rates of relapse but increased rates of GVHD under the Beijing Protocol. This study not only shed light on donor selection by using one modality (the Beijing Protocol) to answer the universal question of HIDs versus URDs, but was also of practical significance due to possible shortage of unrelated donors, sibling donors and other suitable HIDs, especially in contemporary China with the one family one kid policy.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal